Discover What Insurance Covers Wegovy: Your Guide to Coverage and Access


If you’re considering Wegovy for weight management, a crucial question you face is: What insurance covers Wegovy? Coverage of this prescription medication varies widely, depending on your insurer and policy specifics. Major providers such as Blue Cross Blue Shield, Aetna, Cigna, and United Healthcare may include Wegovy coverage under certain conditions. Read on to learn how to navigate insurance plans for Wegovy, what costs you might expect, and tips to maximize your benefits—whether your plan is private, through Medicare Part D, or Medicaid.
Key Takeaways
Insurance coverage for Wegovy varies by provider and plan, potentially affected by FDA approval for cardiovascular benefits, with Medicare Part D and some Medicare Advantage Plans offering coverage.
Out-of-pocket costs for Wegovy can be high, but patients can reduce expenses through prescription discount cards, patient assistance programs, and looking into savings offers by pharmaceutical companies.
Wegovy is approved for chronic weight management in adults and adolescents with obesity or weight-related medical conditions, requiring a reduced calorie diet and physical activity in conjunction, and comes with a significant risk of potential side effects.
Navigating Insurance Coverage for Wegovy
Navigating the complexities of insurance coverage for medications, including Wegovy, can be a daunting task. It is crucial to have a clear grasp of your particular insurance plan and its provisions concerning this medication. The level of coverage for Wegovy can vary widely depending on the insurer – with major providers such as Blue Cross Blue Shield, Aetna, Cigna, and United Healthcare possibly providing benefits. These offerings are subject to change based on variables like plan category and employer-provided options.
Nevertheless, there is cause for optimism. With the FDA’s recent decision to approve additional uses related to cardiovascular health benefits associated with Wegovy, there is an expectation that more comprehensive insurance plans will likely cover it in response. Despite its steep price tag when uninsured, grasping your specific policy details could prove beneficial in taking advantage of broader access facilitated by expanded approvals from regulatory bodies.
Understanding Your Insurance Plan
So, how do you decipher the terms and conditions of your insurance plan? The secret lies in understanding that coverage for Wegovy, an injectable prescription medicine, may vary, and you need to know the specifics of your plan regarding prescription benefits. If you’re enrolled in a Medicare Part D plan, you might have an advantage. Following an FDA decision, these plans can now include prescription drugs like Wegovy in their formularies, opening the doors for individuals with cardiovascular disease to reduce the risk of heart attacks and stroke.
Not just that, some Medicare Advantage plans have already announced Medicare coverage for Wegovy, and others have disclosed planned coverage for 2024. However, the full extent of coverage is still under the wraps. So, a thorough review of your plan’s coverage terms is imperative to ensure you can make the most of your insurance benefits.
Contacting Your Insurance Company
After familiarizing yourself with your insurance plan, the subsequent action is to verify. This can be done by reaching out directly to your insurance company, which involves a simple task: calling the phone number located on the back of your insurance card. Keep in mind that for a Wegovy prescription you may need prior authorization from your healthcare provider. It’s advisable to confirm this requirement with your insurer.
In conversation with your insurance carrier, ensure that you inquire about whether Wegovy needs prior authorization and grasp fully the process for appealing should coverage initially not be granted. Having these details at hand simplifies traversing through the complexities of dealing with insurance matters!
Estimating Costs and Savings Opportunities

Insurance coverage plays a crucial role in managing the expenses associated with obesity treatment. Comprehending both out-of-pocket costs and possible savings when considering medications such as Wegovy is essential. Without insurance, the cost for four 0.75 ml Wegovy pens can reach $1,349.02. The cost you may incur if insured will depend on your particular health insurance plan’s details, which might involve varying deductibles, copayment amounts and classification of medication into specific tiers.
Even though many insurance plans offer coverage for obesity management treatments like Wegovy, they often stipulate certain conditions that must be met before covering these treatments. Thus resulting in a broad spectrum of copay amounts among different users seeking this kind of medical intervention to address their obesity concerns. It is important not to be discouraged by these financial figures, but instead make it a priority to discuss various options available for weight loss medication with healthcare professionals or insurers—to devise strategies that could mitigate these expenses including:
Direct out-of-pocket payments
Copays requirements
Leveraging prescription discount cards
Exploring patient assistance programs
In what follows, we’ll explore each mentioned avenue designed to manage expenditures while pursuing effective obesity management through medicational means.
Out-of-Pocket Costs and Copays
When estimating expenses for any medication, it is important to take into account out-of-pocket costs. Without coverage from health insurance, the price tag for a 28-day supply of Wegovy can hit approximately $1,349.02 – that’s close to $337.25 each week or roughly around $17,585 over a full year. But with insurance coming into play, these expenses may reduce considerably based on your plan’s specific copays and deductible stipulations.
To the cost of Wegovy itself, one should not overlook the expense associated with doctor visits, which can affect overall out-of-pocket spending. The initial visit could set you back between $49 and $129 while follow-up appointments might range from $99 up to about $149 monthly — all contributing factors in calculating total costs when using this medication. Purchasing a longer 90-day supply might be more economical subject to pharmacy pricing structures that are available.
Utilizing Prescription Discount Cards
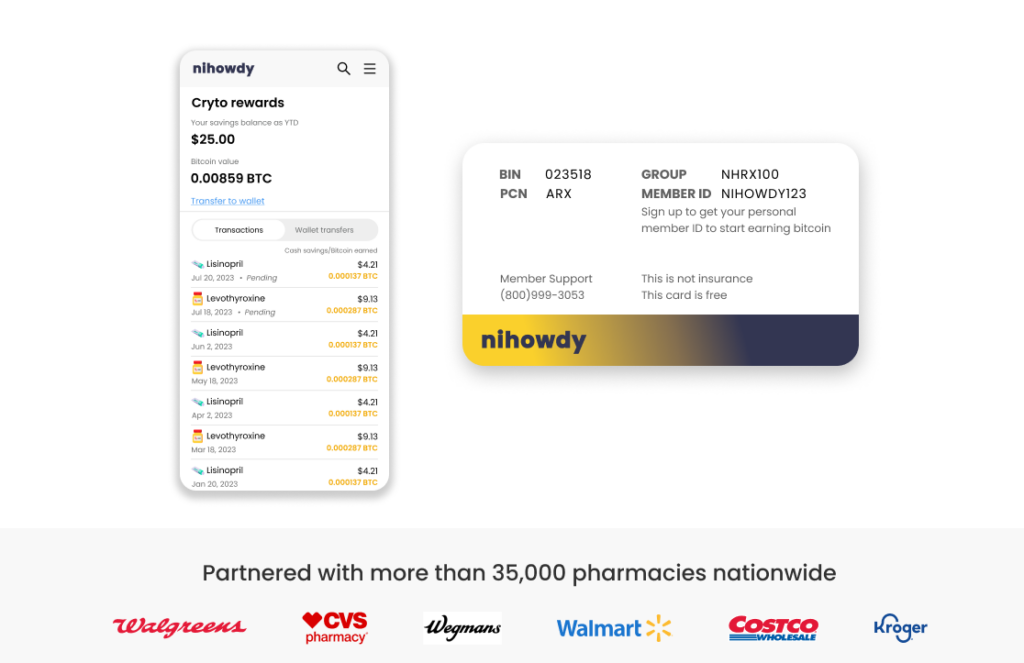
Prescription discount cards are a significant tool in cost management. Consider the case of NiHowdy. They present a leading-edge prescription discount card which rewards users with as much as 3% back in Bitcoin on every purchase made for prescriptions. This not only provides savings on immediate costs, but also gives the advantage of earning incentives at the same time.
The Bitcoin earned through using NiHowdy’s card carries the possibility of increasing in value over time, potentially enhancing one’s financial position. Over an extended period, such growth could help counterbalance escalating healthcare expenses and assist with managing other important life expenditures. Surely this represents a scenario where both savings and earnings go hand in hand.
Patient Assistance Programs and Coupons
Managing expenses extends beyond just insurance coverage and the use of discount cards. Programs for patient assistance and various coupons can considerably ease the financial burden on patients. Offers designed to save money on Wegovy aim to reduce treatment costs, making this medication more accessible.
The savings initiative by Novo Nordisk offers substantial reductions in expenses related to Wegovy—up to $225 for individuals with commercial insurance, and a reduction reaching $500 for those without any form of insurance or who pay directly from their pockets. Patients meeting eligibility criteria may benefit from using the Savings Card specific to Wegovy, which helps lower prescription costs further. If someone is experiencing financial difficulties or doesn’t have health insurance coverage, there are programs available that could provide them access to Wegovy at a significantly reduced cost or potentially free-of-charge.
Wegovy Eligibility and Usage
Recognizing the intricacies of insurance coverage and effective cost management is vital, but equally critical is understanding who qualifies for Wegovy usage and its application. Approved for use by adults as well as adolescents over 12 years old, Wegovy serves as a treatment option within chronic weight management programs. It’s designated specifically for those with obesity or overweight status accompanied by additional health concerns, to be used in tandem with both a reduced calorie diet plan and enhanced physical activity routines.
The question remains on how individuals determine their eligibility for this medication. And once confirmed eligible, what are the steps to effectively incorporate it into an existing weight management strategy? These points merit exploration to ensure comprehensive obesity care planning.
Approved Patient Population
The FDA has approved Wegovy for individuals struggling with weight management due to excess body weight. This approval applies when the individual’s BMI is 27kg/m2 or above in conjunction with at least one weight-related medical condition such as heart disease, or a BMI of 30kg/m2 without any other conditions. For an adult to be eligible for insurance coverage on Wegovy, they must have a BMI of either 30 and over, or at least 27 with an associated health issue related to their weight.
Wegovy holds the green light for long-term treatment of obesity and overweight status among adults — which accounts for roughly 70% of the adult population in America. Coverage extends under certain conditions. Specifically, children aged twelve years old and up qualify if their BMI lies at or beyond the sex- and age-specific 95th percentile.
Integrating Wegovy into Obesity Management
If you qualify for the use of Wegovy, it’s essential to incorporate this medication into your regimen dedicated to managing obesity. Known generically as Semaglutide and commercially available as Wegovy, when paired with a nutritious diet and consistent exercise, it can dramatically aid in shedding extra pounds. This strategic approach may also diminish the likelihood of developing persistent health conditions like cancer, diabetes, and heart disease commonly associated with carrying excess body weight.
For those employing Wegovy among their chosen weight loss medications, adopting an eating plan rich in proteins, fiber-packed foods and abundant nutrients is recommended to boost satiety levels aiding continual weight management efforts. Alongside pharmacological intervention to reduce additional body mass, integrating aerobic exercises alongside strength training activities enhances the drug’s slimming effects. For optimal results while on Wegovy therapy, adherence should be maintained by curtailing consumption of highly processed foods alongside sugary beverages plus limiting alcohol intake. Dietary fats should be predominantly unsaturated sources—monitoring fluid uptake remains crucial not just for quenching thirst but also for helping regulate appetite during one’s journey toward effective obesity control.
Potential Risks and Side Effects of Wegovy

Prior to embracing Wegovy as a treatment option, recognizing the associated health risks and adverse effects is crucial. Notable serious health concerns connected with the use of wegovy include:
Thyroid tumors which could be cancerous, particularly in patients with a past history of specific endocrine conditions
Intense allergic responses
An elevation in heart rate
A variety of other important medical issues
It’s imperative to have an informed conversation about Wegovy with healthcare professionals. This discussion should cover its potential impact on any current medication regimes, especially those for diabetes management, so as to avoid harmful drug interactions.
During the SELECT trial study, approximately one-third (33%) of participants encountered significant side effects from using Wegovy. Such side effects led nearly 17% of individuals participating in the trial to stop taking it altogether due to these negative experiences. Some additional risks that accompany this treatment are chances for developing pancreatitis or gallbladder complications that may necessitate surgical intervention, renal failure, and vision changes among diabetic patients. And heightened susceptibility towards suicidal ideation or behaviors.
Common Side Effects
Despite the potential worry surrounding significant adverse reactions, recognizing the usual side effects associated with Wegovy is crucial. Common gastrointestinal discomforts noted by individuals in the SELECT study encompassed symptoms such as nausea, diarrhea, constipation, and vomiting. Some experienced headaches and fatigue linked to central nervous system effects.
Endocrine-related issues were detected too. Notably low blood sugar was a possible consequence of taking Wegovy. Beyond these frequently documented gastrointestinal effects, other general abdominal problems may occur. Being informed about these potential side effects equips you with better strategies for handling them should they manifest.
Major Cardiovascular Events
Wegovy offers an optimistic outlook for those with higher chances of experiencing a heart attack, stroke, or cardiac-related mortality by potentially diminishing these risks. Its FDA endorsement stemming from cardiovascular advantages could lead to its favored prescription for individuals who are dealing with obesity alongside heart disease.
Acknowledging the possibility of adverse reactions is crucial. Wegovy’s advantages transcend mere weight management. It presents a holistic approach to assist individuals contending with not only obesity but also accompanying health issues linked to their weight.
Medicare and Medicaid Coverage for Wegovy
In the conversation about insurance coverage for Wegovy, it’s crucial to recognize not just private insurers but also the role played by Medicare and Medicaid. Although excluded from Medicare coverage, state-based Medicaid programs may provide differing levels of government coverage, with some states extending either limited or comprehensive inclusion.
For those enrolled in Medicare Part D plans, expenses linked to medications such as Wegovy can come with an assortment of shared costs — including monthly premiums and deductibles along with coinsurance fees — leading up to out-of-pocket expenses that might fluctuate between $325 and $430 each month until they hit their yearly threshold for drug expenditures. There is a silver lining: if incorporated into Medicare Part D plans’ formulary offerings, beneficiaries who are overweight or obese and suffer from cardiovascular diseases could access this medication under their coverage benefits—an alteration which has implications on overall Medicare expenditures.
Medicare Advantage Plans and Medigap Policies
Should you be a participant in a Medicare Advantage Plan or possess Medigap insurance, the coverage for Wegovy might pique your interest. Under Medicare, Medicare is not required. Part D plans, it is possible that Wegovy is categorized as a drug within the specialty tier, which may result in increased coinsurance expenses.
The degree to which Medicare Part D schemes provide coverage for Wegovy and impose limitations like prior authorization prerequisites will have an impact on its accessibility and utilization by those who are eligible. Consequently, it’s essential to comprehensively grasp the details of your particular Medicare policy’s provisions.
State Medicaid Coverage
Coverage for Wegovy under Medicaid varies from state to state, with some providing coverage under specific conditions and others possibly not offering coverage at all. Patients should reach out directly to their respective state Medicaid office to get accurate information about the coverage of Wegovy, as each has distinct policies and guidelines in place.
Factors that could affect a state’s decision on whether or not to cover Wegovy through its Medicaid program include:
The perceived value for money of the medication
Its presence on the preferred drug list within that state
The necessity of prescribing it after conducting differential diagnosis
Leveraging online resources can empower you with guidance when seeking insight into your medicaid benefits and understanding how they might pertain to obtaining coverage for government.
Summary
Understanding your insurance plan thoroughly, along with being aware of cost management strategies such as prescription discount cards and patient assistance programs, can significantly ease the process of figuring out coverage and costs for a new medication like Wegovy. It’s important to be well-informed about eligibility requirements, potential risks, and side effects when making decisions regarding your health. Coverage for Wegovy under Medicare or Medicaid may differ. Thus, familiarizing yourself with the specific terms and conditions of your insurance is crucial. Equipped with these insights, you’re in a strong position to confidently manage your health care journey involving Wegovy.
Frequently Asked Questions
Is Wegovy covered by insurance?
The availability of coverage for Wegovy can differ from one insurance company to another, hence it is crucial to reach out to your insurer directly in order to ascertain whether they provide coverage for this medication.
To determine if Wegovy falls under the scope of your benefits, contacting your insurance company directly would be the advisable course of action.
How can I manage the costs associated with Wegovy?
You can manage Wegovy costs by using prescription discount cards like NiHowdy and seeking assistance from patient support programs. This can help alleviate out-of-pocket expenses and copays.
Who is eligible to use Wegovy?
Adults and adolescents aged 12 years and older are eligible for Wegovy, which is designed for chronic weight management. Eligibility also depends on meeting certain BMI criteria as well as having health conditions related to weight.
What are the potential side effects of Wegovy?
It is important to converse with your healthcare provider about any worries you might have as wegovy may pose significant health dangers, such as thyroid tumors, allergic reactions, and pancreatitis. More prevalent side effects including digestive problems and headaches can occur.
Does Medicare or Medicaid cover Wegovy?
Medicare does not include coverage for Wegovy.
On the other hand, whether Medicaid covers Wegovy can differ from state to state. To determine if you have coverage for Wegovy under Medicaid, it is advisable to reach out directly to your specific state’s Medicaid office.