Does Methadone Get You High? Understanding its Effects and Misconceptions
Does Methadone Get You High? Understanding its Effects and Misconceptions


Many wonder, ‘Does methadone get you high?’ To put it plainly, no, it doesn’t. This article delves into why methadone, a medication that’s key in treating opioid addiction, lacks the high of other opioids, and how it’s used effectively in maintenance therapy.
Key Takeaways
Methadone is used in treating opioid dependence and binds to opioid receptors in the brain without inducing a euphoric high, which helps manage cravings and withdrawal symptoms.
While methadone reduces withdrawal discomfort and blocks the euphoric effects of other opioids, there is a real risk of overdose which requires carefully managed dosages and medical supervision.
Despite common misconceptions, methadone does not cause damage to vital organs or addiction when prescribed, and withdrawal is manageable with proper medical guidance.
Unraveling the High: Does Methadone Induce Euphoria?

Methadone is a synthetic opioid that plays an essential role in treating addiction to opioids. While it activates the same opioid receptors as other addictive opioids, methadone does not evoke the euphoric sensation they do when taken at therapeutic levels. Despite its effectiveness, there is a potential for methadone addiction, especially when not used as prescribed, highlighting its ability to produce euphoria and its potential for misuse and diversion among those with a high tolerance to opioids and those who are not dependent on them. Specially certified providers and facilities, under the oversight of the Substance Abuse and Mental Health Services Administration (SAMHSA), play a crucial role in reducing the potential for methadone misuse by ensuring its proper administration and regulation.
For those struggling with an opioid use disorder, this feature of methadone proves advantageous by curbing cravings and mitigating withdrawal symptoms without luring users into seeking a high. Methadone effectively sustains recovery efforts while keeping the brain’s opioid receptors occupied, which facilitates the transition away from dependency on opioids.
It’s important to understand that treatment involving methadone isn’t about exchanging one addiction for another. Rather it serves as a means for patients to reclaim their lives from their ongoing obsession with opioids and move forward in overcoming their addictions. The ultimate objective of employing methadone within treatments is helping individuals escape the grip of such dependencies, not fostering new ones.
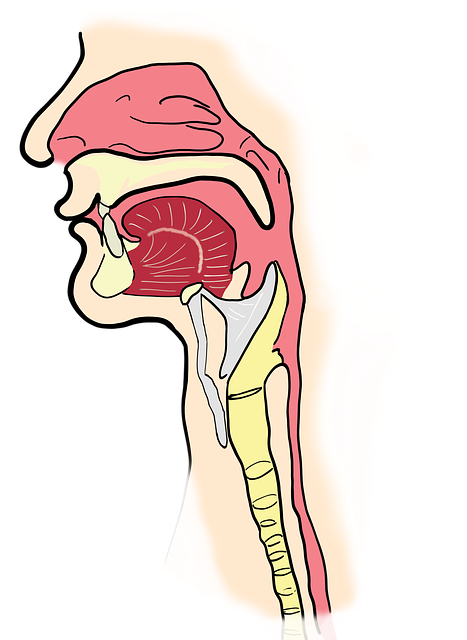
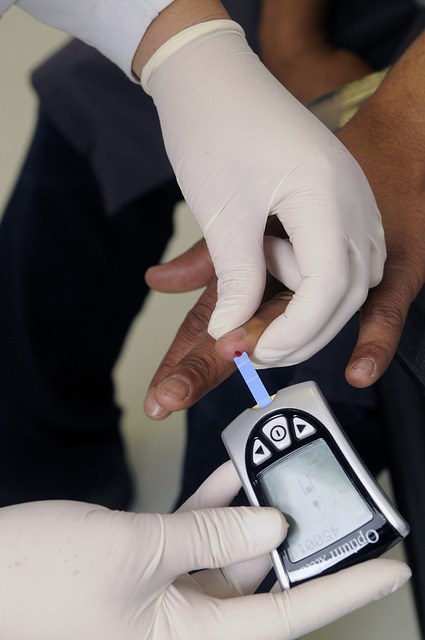
The Mechanism of Methadone in Opioid Treatment Programs

Understanding the role of methadone in opioid treatment programs requires knowledge of its action within the human body. Methadone, which is an opioid agonist:
Attaches to the same neuronal receptors targeted by other opioids
Accomplishes this without inducing euphoria
Effectively alleviates cravings and wards off symptoms associated with withdrawal
Allows individuals undergoing treatment to maintain a normal lifestyle devoid of the overpowering urge to consume opioids
Is prescribed to prevent withdrawal symptoms and manage opioid withdrawal, highlighting its effectiveness in reducing opioid cravings and withdrawal symptoms, and its role in preventing opioid overdose.
Methadone’s impact on modifying how both the brain and nervous system perceive pain is also crucial. It eases discomfort associated with withdrawal while simultaneously blocking out the highs derived from using substances like heroin, thus acting as a protective barrier for those who are recovering. There exists a genuine danger concerning overdosing on methadone. Hence why precise dosing under medical supervision is essential. The challenges and regulations around how doctors prescribe methadone for opioid treatment programs underscore the strict prescriber regulations and the effectiveness of methadone compared to other medications. The Substance Abuse and Mental Health Services Administration (SAMHSA) plays a pivotal role in certifying providers and overseeing these regulations, ensuring that methadone treatment programs meet the necessary standards for safety and efficacy.
How Methadone Differs from Other Opioids
What sets methadone apart from other opioids is its ability to alleviate cravings and withdrawal symptoms over an extended period while not inducing the euphoria that shorter-acting opioids typically do. As a long-acting opioid agonist, it operates differently by preventing the pleasurable sensations often sought after in opioid use.
Because methadone does not produce a significant ‘high,’ it has a lower potential for recreational misuse. This unique attribute enhances its suitability as an effective agent in maintenance treatment programs, distinguishing it from other types of opioids and highlighting its role in opioid addiction therapy.
Methadone Maintenance Treatment: A Balancing Act
Methadone maintenance treatment demands a precise balance. Patients are administered specifically calibrated doses that aim to fend off withdrawal symptoms while avoiding the risk of experiencing euphoria from the medication. This careful adjustment starts under strict supervision by healthcare providers, who monitor and modify initial dosing based on how each patient’s body reacts.
With time and demonstrated stability in their condition, patients may be granted take-home doses for management between visits to the clinic. Such provision is essential in allowing them continual support with their therapy even when they are not present at the medical facility. In the absence of this maintenance treatment, those withdrawing from opioids could start exhibiting methadone withdrawal indicators within 36 hours post-last opioid intake. These discomforts might continue for over two weeks, thus intensifying obstacles faced during opioid detoxification and recovery processes.
The Reality of Methadone Use and Potential Side Effects

All drugs, including methadone, carry the potential for side effects. Some individuals may experience issues such as sedation or sexual dysfunction when on this medication. Due to methadone’s extended half-life, there can be an accumulation of the drug in one’s body over time. This accumulation heightens the risk of overdosing, especially among those who do not routinely consume opioids. Because methadone’s peak respiratory depressant effects outlast its analgesic properties, there is an increased danger of breathing suppression.
Nevertheless, it’s important to note that adverse effects like nausea can often be mitigated by adjusting the dosage level. When dosed therapeutically and managed correctly without exceeding prescribed amounts — typically providing pain relief lasting between four and eight hours — methadone does not cause euphoria nor pose a safety threat leading to intoxication.
For women who are pregnant or breastfeeding, additional precautions should be taken into consideration about methadone treatment. While it has been found capable of crossing into both placenta and breast milk, potentially inducing withdrawal symptoms in newborns after birth—the risks associated with withdrawing from heroin appear more severe, making methadones’ benefits during management outweigh these concerns.
Methadone Overdose Risks Without the High

Methadone plays an essential role in the management of opioid use disorder, but it also carries significant risks. Life-threatening situations can arise from a methadone overdose when combined with alcohol or other drugs. It’s imperative that patients strictly follow prescribed dosages and exercise caution by abstaining from alcohol and remaining vigilant while driving or using machinery to mitigate the risk of overdose.
While methadone represents just a small proportion of overall opioid prescriptions, its connection to a disproportionate number of fatalities linked to opioid overdoses is concerning. This highlights the critical need for diligent application of methadone treatments and rigorous medical oversight when clinicians prescribe this drug as part of addiction therapy to curb potential drug abuse and forestall developing an addiction to methadone itself.
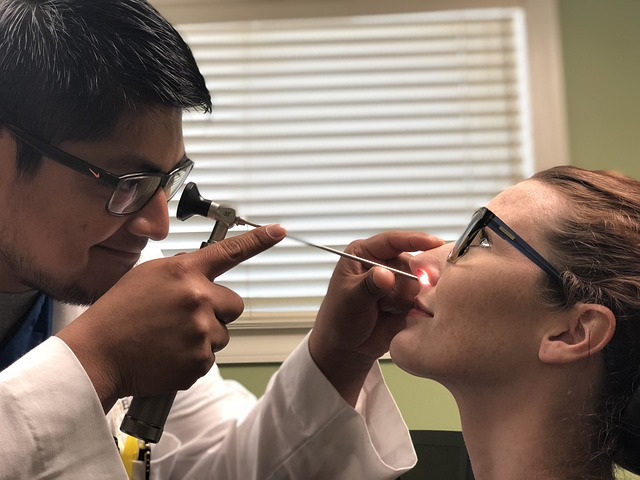
Navigating Methadone Treatment for Opioid Use Disorder (OUD)
Initiating methadone treatment for opioid use disorder, a form of narcotic addiction is not an easy process. It demands adherence to a well-defined and carefully structured treatment plan under the supervision of medical professionals. As one of the most secure and efficacious methods for treating opioid addiction, methadone has been found instrumental in reducing fatal overdose risks while assisting individuals on their journey toward recovery by controlling withdrawal symptoms and curbing cravings.
Obtaining access to methadone can present obstacles due to societal stigma surrounding its use, regulatory barriers, and scarcity of available treatment programs. Despite these challenges, if those with opioid dependency can secure such treatments —methadone can considerably enhance life quality — providing significant support on their path towards overcoming addiction.
The Role of Mental Health Services in Methadone Treatment
The administration of mental health services, notably through the Substance Abuse and Mental Health Services Administration (SAMHSA), plays an integral role in the delivery of methadone treatment. SAMHSA certifies providers and facilities for dispensing methadone as part of a comprehensive treatment plan, offering essential support to manage not only physical dependency but also the psychological facets of substance abuse. This integrated strategy combines medication-assisted therapy with vital counseling and support networks to suppress addiction symptoms. Counseling sessions serve as a foundation for emotional regulation, bolstering social reinforcement and empowering patients to tackle both their substance abuse issues and concurrent mental health challenges by:
Fortifying their social ties
Cultivating strategies for resilience
Establishing and pursuing personal aspirations
Professionals skilled in addiction treatment within the realm of mental health are equipped with the specialized knowledge necessary for addressing accompanying psychiatric conditions. By attending to both bodily dependencies and psychological well-being concurrently, this holistic method substantially amplifies the success rates associated with methadone-based therapies.
The Journey to Recovery: Take-home Doses and Clinic Visits
The path to recovery often starts with regular clinic appointments for the administration of medication and oversight. As individuals prove consistent in following their treatment plan, they may be eligible for take-home doses—a critical advancement in their journey toward rehabilitation that signals a move toward autonomy and everyday life normalization.
Eligibility for receiving take-home prescriptions of a Schedule II drug is contingent upon patients demonstrating stability while under medical care. The stipulation mandates readiness on the part of the patient to responsibly handle their medication when away from clinical support, fostering continued strides toward healing.
Financial Considerations in Methadone Treatment
Methadone treatment encompasses more than just the physical and emotional recovery aspects. Economic considerations are also crucial. Many individuals find the cost associated with methadone treatment to be a formidable barrier. Nevertheless, organizations such as Nihowdy alleviate this burden by providing a prescription discount card renowned for its top-notch services and straightforward pricing structure, facilitating discounts and price comparisons at various pharmacies.
By taking advantage of Nihowdy’s prescription discount card, users can typically expect savings up to 20% on brand-name drugs and up to 40% on generic medications. Using Nihowdy’s service extends benefits beyond instant cost reductions. Every time customers refill their prescriptions using the card, they have an opportunity to accumulate Bitcoin rewards that amount to up to 3%, presenting an additional monetary incentive.
Long-Term Savings with Nihowdy
The prospect of accruing savings through Bitcoin is rooted in the possibility of sustained financial appreciation. By utilizing Nihowdy’s prescription discount card, individuals have the opportunity to garner Bitcoin rewards progressively. Such gradual accrual can offset healthcare costs and other substantial fiscal duties over time.
Cardholders are entitled to receive up to an extra 3% back in Bitcoin for every prescription purchase made. The anticipated increase in value of these Bitcoin incentives from Nihowdy could amplify total savings enjoyed by users of the card. This distinctive aspect provides enduring economic advantages that surpass just instant discounts on medication purchases.
Methadone Myths Debunked

We have explored the world of methadone treatment and clarified several false beliefs. Contrary to a prevalent fallacy, methadone does not cause addiction. Instead, it is a medically prescribed intervention for opioid use disorder that assists individuals in maintaining normalcy in their lives.
Concerns about methadone harming critical organs are unfounded. When used as directed by medical professionals, long-term consumption of this medication does not harm major organs like the liver or kidneys. The allegations suggesting that methadone leads to bone and teeth degradation or directly induces weight gain are also baseless myths. While it may lead to dry mouth necessitating diligent dental care, it’s not responsible for the direct deterioration of bones or teeth. If patients experience weight increase while on this treatment, it tends to be due to overall better health status and heightened appetite rather than the medicine itself.
Lastly, there exists a misconception that withdrawing from methadone is unmanageable — yet another myth we can dispel here today. With appropriate clinical oversight, withdrawal symptoms often present more slowly compared with those stemming from other opioids, ensuring manageability when discontinuing its use properly. Dismantling these misguided notions surrounding Methadone collectively facilitates conversations around opioid use disorder treatments grounded in knowledge sensitivity compassion.
Summary
Methadone, an artificial opioid agonist, is essential in the management of opioid use disorder. It mitigates cravings and withdrawal symptoms by attaching to the same neurological receptors as other opioids but does not produce euphoria. This characteristic differentiates it from other opioids and contributes to its effectiveness in recovery since methadone’s extended duration reduces its potential for abuse.
There are hazards associated with methadone treatment, such as the possibility of a life-threatening overdose if combined with additional substances. Adherence to precise dosing instructions and careful monitoring by healthcare providers can control these dangers effectively. When coupled with Nihowdy’s discount card offering financial advantages, this method of treatment becomes a cost-effective option that provides substantial help for individuals struggling with addiction to opioids.
Frequently Asked Questions
Does methadone make you high?
When administered at dosages prescribed for treatment, methadone does not induce a high. It engages with the brain’s opioid receptors yet fails to elicit feelings of euphoria.
How does methadone differ from other opioids?
Methadone stands out among opioids as a long-acting agonist that not only diminishes cravings and withdrawal symptoms but also does so without eliciting euphoria. It delivers more consistent opioid effects relative to other opioids.
Are there risks associated with methadone treatment?
Certainly, while methadone treatment does carry risks like the possibility of a life-threatening overdose, especially if mixed with other substances, these dangers can be mitigated through strict compliance with prescribed dosages and under medical oversight.
What are some common myths about methadone?
Disregard the unfounded myths suggesting that methadone causes addiction, harms organs, results in bone and dental issues, or triggers weight gain. There is no scientific proof to back up these false beliefs.
Can I save on my methadone treatment with a discount card?
Certainly, utilizing a prescription discount card like Nihowdy’s can reduce the cost of your methadone treatment and provide you with rewards.
Does Methadone Get You High? Understanding its Effects and Misconceptions Read More »