Understanding Drug Interactions: Can You Take Atorvastatin with Amoxicillin Safely?
Understanding Drug Interactions: Can You Take Atorvastatin with Amoxicillin Safely?


If you’re juggling prescriptions for atorvastatin and amoxicillin, safety naturally comes to mind. Can you take these medications together without risk? This article gives you a straightforward look into “Can you take atorvastatin with amoxicillin” and whether they can be taken safely together, cutting through medical jargon to the clarity you need.
Key Takeaways
Atorvastatin is a cholesterol-lowering medication with potential side effects such as muscle pain, which could indicate serious conditions like liver damage or rhabdomyolysis, while Amoxicillin is an antibiotic used for bacterial infections that can cause gastrointestinal upset and skin reactions.
There are no documented drug interactions between Atorvastatin and Amoxicillin, which generally means they can be used together safely, but patients should always consult healthcare providers for personalized advice.
Alternative medications are available for patients who experience side effects or have contraindications with Atorvastatin or Amoxicillin, such as Fibrates, Omega-3 fatty acids, Metronidazole, and Azithromycin, and the choice should be tailored to the patient’s individual health needs.
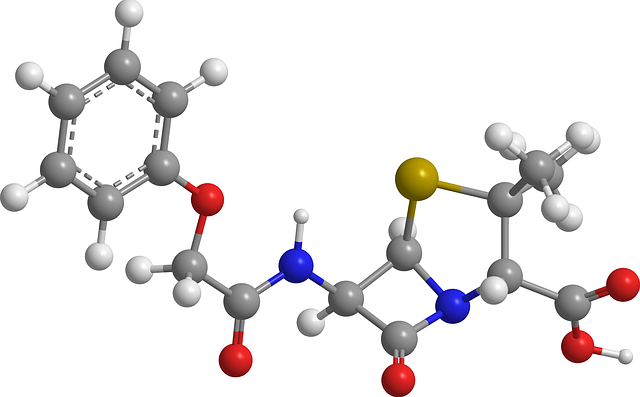
Atorvastatin and Amoxicillin Overview
Atorvastatin is a vital medication employed to lower cholesterol and triglyceride levels in the blood by dietary adjustments, thereby aiding in the prevention of heart complications such as angina, myocardial infarction, or strokes resulting from occluded vessels. Nevertheless, its use does not come without drawbacks. Typical adverse effects associated with Atorvastatin may include headaches, voice changes including hoarseness, facial pain around the eyes and cheekbones, along with discomfort during urination.
Conversely, Amoxicillin acts like a protective warrior against bacterial invasions. By obstructing cell wall formation in vulnerable bacteria strains it effectively treats infections affecting various body parts.
ears
nasal passages
pharyngeal region
urinary system
dermis
Yet this gallant defender isn’t flawless. Common side effects linked to Amoxicillin include digestive upsets manifesting as nausea or vomiting and diarrhea – some individuals might also experience skin rashes.
To ensure your treatment remains safe and efficient, it requires vigilance regarding potential drug interactions that can occur between these medications, including food-related influences on their efficacy. With that preamble addressed, let us now scrutinize more closely the individual profiles of each substance before examining how they might interrelate within your therapy regimen.
Atorvastatin
Taking atorvastatin, a medication known for inhibiting the enzyme HMG-CoA reductase, which is crucial in cholesterol synthesis, effectively reduces levels of bad lipids and proteins in our bloodstream. This drug acts as an ally against elevated cholesterol, similar to how superheroes combat villains.
Individuals using atorvastatin have sometimes presented with various symptoms such as:
Fever
Joint pain or swelling unusual bleeding or bruising
Rashes on the skin
Diminished appetite
Fatigue
Nausea
Such manifestations may be indicative of potential liver damage. Those administered atorvastatin who notice any abnormalities should promptly heed these signs. Take John’s case: his wife Sarah noticed him developing jaundice-like symptoms. Fortunately, her insistence on medical consultation led to timely treatment after discovering it was indeed indicating hepatic impairment.
It’s imperative to watch out for unexplained muscle pain tenderness or weakness if you’ve been prescribed atorvastatin—particularly when accompanied by fever dark colored urine could signal a rare but serious condition called rhabdomyolysis that involves the breakdown of skeletal muscle tissue potentially leading kidney damage even death Jane serves example not ignoring bodily distress signals—an avid exerciser she initially mistook increasing discomfort typical workout soreness It wasn’t until enduring excruciating agony that she sought aid and learned about onset rhabdomyolysis. Thankfully due to prompt care, she fully recovered.
In essence, when undergoing treatment with drugs like Atorvastatin vigilance remains critical to monitor unexpected changes in your health status and contacting providers swiftly upon noticing anything extraordinary.
Amoxicillin
Shifting focus to Amoxicillin, this antibiotic stands as a formidable opponent against various bacterial infections. It is highly effective in combating ailments of the ear, nose, throat, urinary system, and skin. Even an efficient combatant like Amoxicillin must confront its challenges.
Amoxicillin usage often comes with some typical side effects that can manifest as digestive issues including nausea and diarrhea or result in skin rashes for certain individuals. Consider Bob’s experience. While taking Amoxicillin during his daughter’s graduation day festivities, he was compelled to spend more time seeking solace in the bathroom than celebrating due to these adverse reactions.
There is a silver lining when it comes to administering Amoxicillin—it boasts excellent absorption through the gastrointestinal tract without being heavily influenced by food consumption. Thus patients have the flexibility of ingesting it on either full or empty stomachs—a convenience many appreciate.
The body eliminates most of this drug unchanged via urine, which means kidney health plays a pivotal role in its processing within our systems. As evidenced by Susan who continued her regimen of ample water drinking and proper nutrition while medicated with Amoxicillin—actions that supported her renal health allowing for effective management and removal of the medication from her body.
Drug Interaction between Atorvastatin and Amoxicillin
Having examined both Atorvastatin and Amoxicillin as separate entities, we can now address the potential for drug interactions between them. Fortunately, no known drug interactions have been recorded when these two medications are used concurrently. Consequently, they are typically deemed safe to be administered in tandem without any anticipated issues from their combination.
Nevertheless, even with a lack of documented interactions between Atorvastatin and Amoxicillin, one should not initiate co-administration without medical counsel. Imagine opting for a bespoke suit. It’s meticulously crafted to your measurements ensuring an impeccable fit. Likewise, health professionals provide advice that’s specifically tailored to align with your individual health needs and medical history.
It is important to bear in mind that the absence of evidence is not evidence of absence regarding drug-drug interactions. Vigilance remains paramount, erring on the side of caution often precludes unforeseen complications associated with taking multiple drugs simultaneously. Indeed, “prevention is better than cure,” isn’t it?
How Atorvastatin and Amoxicillin Affect Each Other
It has been determined that Atorvastatin and Amoxicillin do not interact in a way that has been documented.
Should you be administered Atorvastatin in tandem with Amoxicillin, you could observe symptoms including:
headache
feelings of dizziness
sensations of lightheadedness
potential fainting spells
alterations in your pulse or cardiac rhythm
These manifestations could stem from the cumulative effect. Yet there’s no cause for immediate concern or reason to add undue worry to your plate.
Current evidence does not point towards any significant influence on the efficacy of either drug due to their simultaneous consumption. In other words, while some side effects might manifest, each drug seems capable of maintaining its effectiveness unimpeded by the presence of the other – akin to two different melodies blending without discordance.
Safety Precautions for Combining Atorvastatin and Amoxicillin
Understanding the potential effects and interactions of medications is crucial. Equally important is being aware of safety measures and possible risks associated with their use. When taking atorvastatin in combination with amoxicillin, particular attention should be paid to older patients who face a higher risk for muscle damage and hospitalization.
Nonspecific signs like muscular pain or kidney issues could point toward statin toxicity but are often misconstrued as less serious conditions, underscoring the importance of vigilance and keeping your healthcare provider informed about any changes in your symptoms.
To minimize the risk of side effects while on statins, consider alternative antibiotics or suspending statin usage during antibiotic treatment under medical supervision. This decision shouldn’t be made independently. It’s essential not to alter medications without first talking over options with a healthcare professional regarding all drugs currently used, including both statins and antibiotics.
The usual starting dose for atorvastatin is 10 mg but may require adjustment if taken alongside antibiotics such as amoxicillin. The goal is always to strike an optimal balance that safeguards one’s health outcomes effectively.
When to Consult Your Healthcare Provider

If you find yourself uncertain about when to contact your healthcare provider, be assured that it is appropriate to do so anytime confusion arises. Even in the absence of recognized drug interactions between Atorvastatin and Amoxicillin, seeking advice from medical professionals for assurance is recommended.
Should you notice any out-of-the-ordinary health changes, it’s crucial to obtain immediate care. Be vigilant for symptoms such as:
unexplained discomfort or pain in muscles
joint pain or swelling
unusual bleeding or bruising
skin rash
itching
loss of appetite
fatigue
nausea
vomiting
dark colored urine
onset of fever chills
Do not overlook therapeutic duplication warnings. These are particularly significant during daytime hours which call for heightened vigilance.
Always keep in mind the importance of prioritizing your well-being and erring on the side of caution.
Alternative Medications
If Atorvastatin or Amoxicillin is not a good fit for you, possibly due to adverse effects, there’s no need to worry as substitute drugs exist. Should you require an alternative for Atorvastatin because of unsuitability or side effects, these options may be considered.
Fibrates: Beneficial in managing atherogenic dyslipidemia and particularly useful when high triglycerides and low HDL-C levels are present.
Bile acid sequestrants: Drugs like cholestyramine, colestipol, and colesevelam can reduce LDL cholesterol by hindering the absorption of bile acids.
Omega-3 fatty acids: These supplements aid in cutting down triglyceride levels, which might help prevent the development of atherosclerosis.
Ezetimibe: A choice that impedes cholesterol uptake from the intestines. It is usable alone or alongside statins.
Alternatively, for Amoxicillin intolerance or contraindication cases involving potential drug interactions when taking atorvastatin with this antibiotic – Metronidazole stands out as another option against specific anaerobic bacterial and parasitic infections. Azithromycin also emerges as a safer bet while on statins compared with amoxicillin owing to fewer interaction risks. Nevertheless, consulting your healthcare provider remains vital in pinpointing suitable medication substitutes tailored to personal health circumstances, including careful consideration of any potential drug interactions.
Tips for Managing Medication Interactions
Navigating the complexities of drug interactions can be simplified with certain strategies. Choosing to fill all your prescriptions at one pharmacy allows for a complete record of medications, which helps in detecting potential drug interactions.
Maintaining clear lines of communication with healthcare professionals and pharmacists is vital to fully understand how to take each medication and be aware of any likely interactions. Don’t hesitate—they are there as your partners throughout this process.
It’s important also to consider the interaction between drugs and dietary substances such as vitamins and herbs. An example is that patients taking Atorvastatin need to know about the heightened risk for liver damage and rhabdomyolysis if they consume grapefruit juice while on this medication.
Ultimately, having thorough knowledge regarding why you’re taking each medicine and how it should be taken properly minimizes interaction risks significantly. Being well-informed not only empowers but might very well save lives.
Real-Life Experiences: Patient Stories
Narratives from individuals on the combined regimen of Atorvastatin and Amoxicillin provide insight into their encounters with these medications. Notably, a number of them experienced gastrointestinal discomfort such as bloating and loose stools while taking both drugs concurrently.
In contrast, others have discovered that incorporating Atorvastatin into their medication routine did not hinder the effectiveness of Amoxicillin in treating bacterial infections. Indeed, several accounts highlighted improved cholesterol readings while simultaneously managing an infection with both Atorvastatin and Amoxicillin.
For those who faced adverse effects, healthcare professionals recommended minor adjustments when they took their medicines—strategies that successfully mitigated digestive disturbances. These patient experiences underscore the importance of vigilance and transparent communication with medical practitioners during treatment.
Summary
We’ve taken a deep dive into Atorvastatin and Amoxicillin, understanding their uses, side effects, potential interactions, and safety precautions. It’s clear that while these drugs can generally be used together without expected drug-drug interactions, it’s crucial to consult healthcare providers and stay vigilant to any unusual symptoms.
Remember, each individual’s health journey is unique. So, always communicate openly with your healthcare providers, and don’t hesitate to ask questions. After all, you’re the captain of your ship, and understanding these interactions empowers you to navigate your health journey confidently.
Frequently Asked Questions
Can Atorvastatin and Amoxicillin be taken together?
Indeed, it is usually acceptable to take Atorvastatin and Amoxicillin concurrently. Confirming this with your healthcare provider before doing so remains essential.
What are some common side effects of Atorvastatin and Amoxicillin?
Be mindful of the usual effects associated with taking Atorvastatin, which includes symptoms like headaches, voice hoarseness, and discomfort during urination. Ingestion of Amoxicillin might result in issues such as digestive upset and rashes on the skin.
Are there alternative medications to Atorvastatin and Amoxicillin?
Indeed, for Atorvastatin, there are substitute medications available such as fibrates, bile acid sequestrants, and Omega-3 fatty acids. Metronidazole and Azithromycin serve as alternatives to Amoxicillin.
Before altering any medications you’re taking, you must seek the advice of your healthcare provider.
What precautions should be taken when combining Atorvastatin and Amoxicillin?
Ensure that you carefully watch for any abnormal symptoms when combining Atorvastatin with Amoxicillin, keep a transparent dialogue with your healthcare professional, and adhere to the correct scheduling and taking of the drugs.
How can I manage medication interactions?
To mitigate the risk of adverse drug interactions, it is advisable to consistently use a single pharmacy for filling all prescription medications. Engage in transparent communication with both pharmacists and healthcare professionals, grasp the function of each medication you are taking, and remain aware of any possible interactions with certain foods or beverages.
By adopting these precautions, you can decrease the likelihood of detrimental drug interactions and safeguard your health and safety.
Understanding Drug Interactions: Can You Take Atorvastatin with Amoxicillin Safely? Read More »