Is Ritalin the Same as Adderall? Unpacking the Truth About ADHD Medications
Is Ritalin the Same as Adderall? Unpacking the Truth About ADHD Medications


Is Ritalin the same as Adderall? This is a common and crucial question for anyone dealing with ADHD treatments. Although both Ritalin and Adderall are stimulants designed to help control ADHD symptoms, they are not the same medication. This article delivers a clear, concise analysis of their differences and how they might affect you, guiding you through the decision-making process of selecting the right treatment approach.
Key Takeaways
Ritalin and Adderall are both central nervous system stimulants used for ADHD but they differ in chemical composition and side effects, which can influence individual treatment choices.
Ritalin generally is more effective for children and adolescents, while Adderall is favored for adults, highlighting the importance of personalized treatment plans for ADHD.
Beyond medication efficacy, considerations for choosing between ADHD medications include onset and duration of effects, potential side effects, the individual’s medical history, and response to medication.
Unraveling the ADHD Medication Maze: Ritalin vs. Adderall
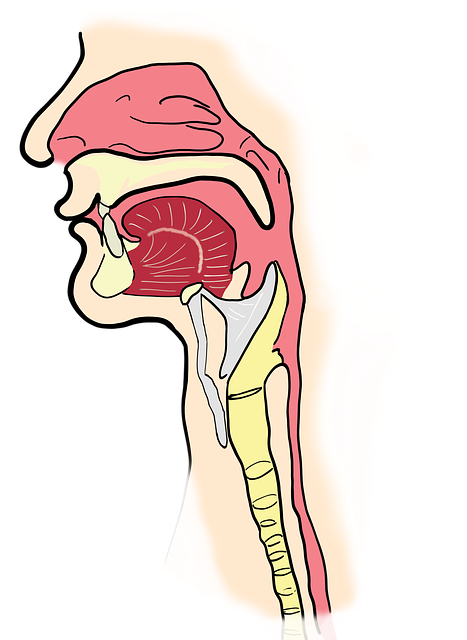
In the intricate realm of ADHD treatments, Ritalin and Adderall stand out as key medications. These central nervous system stimulants are established in their efficacy for mitigating symptoms associated with ADHD by improving communication within the brain, which aids in regulating thoughts, emotions, and actions.
Defining Attention Deficit Hyperactivity Disorder (ADHD)
ADHD, a condition marked by an inability to regulate thoughts, emotions, and actions effectively, is akin to possessing the power of a Ferrari engine in one’s brain paired with the insufficient stopping power of bicycle brakes. Common indicators include difficulty maintaining focus, excessive restlessness, and sudden impulses.
Effective management of ADHD symptoms can greatly enhance productivity and overall quality of life for those affected. A comprehensive approach often involves implementing both medication and behavioral therapy as part of adhd treatment strategies to help individuals cope better with their challenges.
Stimulant Medications in Focus

Ritalin and Adderall operate as stimulant medications by boosting the amounts of neurotransmitters, specifically dopamine and norepinephrine, within the brain. By doing so, they have a significant impact on the central nervous system that enhances alertness, attention span, and energy, which consequently improves concentration while diminishing impulsiveness.
The Core Differences Between Ritalin and Adderall
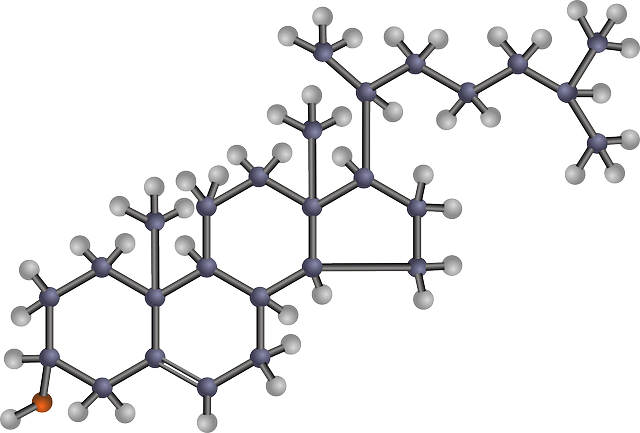
While Ritalin and Adderall share some commonalities, they are not the same. The fundamental distinction between them is rooted in their chemical makeup. Methylphenidate is the active ingredient in Ritalin, whereas Adderall contains a combination of amphetamine salts: amphetamine and dextroamphetamine.
It’s akin to contrasting apples with oranges—they’re both fruits but inherently different from one another.
Chemical Composition Clash: Methylphenidate vs. Amphetamine Dextroamphetamine
Exploring their chemical composition, Ritalin is comprised of methylphenidate and functions by inhibiting the reuptake of neurotransmitters. Adderall, on the other hand, is formulated from amphetamine salts which not only hinder reabsorption but also stimulate the release of these brain chemicals.
The variation in how they work accounts for the unique impacts that each has on neural activity.
Onset and Duration: Timing is Everything

In the realm of medication, when the effects manifest is crucial. Ritalin quickly gets to work, usually within 20 to 30 minutes post-consumption. It’s a fleeting presence with its impact dwindling after merely two to three hours.
On the contrary, taking Adderall can be likened to a long-distance runner due to its gradual onset—it requires about half an hour to one full hour before starting its action—but provides sustained results that endure for as long as 12 hours in extended-release versions.
Comparative Efficacy: Ritalin vs. Adderall
When treating ADHD, it’s not about which one medication is superior, but rather how each medication fits the unique needs of individual patients. Comparing ADHD medications indicates that Ritalin tends to be more beneficial for children and adolescents, whereas Adderall usually proves more effective in adults.
Systematic Review Insights
In 2018, a comprehensive meta-analysis verified the variations in efficacy depending on age. The study determined that for ADHD in children or adolescents, methylphenidate—which is the primary component of Ritalin—proved to be most beneficial.
On the other hand, amphetamines like Adderall emerged as the superior treatment option for adult patients suffering from ADHD.
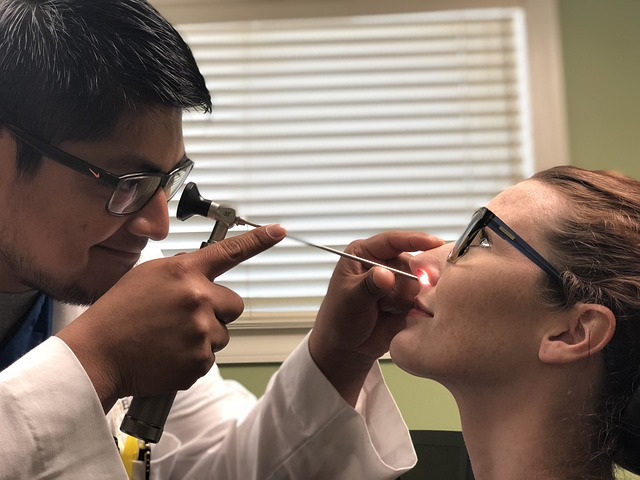
Personalizing ADHD Treatment: One Medication Doesn’t Fit All
Deciding whether to use Ritalin or Adderall is a highly personalized process. It demands an in-depth assessment of one’s unique needs, health background, and how they react to each drug. Adults with ADHD might consider alternative non-pharmacological strategies as part of their management plan including:
Cognitive behavioral therapy
Regular exercise and physical activity
Practicing mindfulness and meditation
Modifying dietary habits
Using herbal supplements
Collaborating closely with a healthcare provider is crucial for establishing the most effective treatment regimen.
The paramount objective is to identify the optimal therapeutic approach tailored specifically for you!
Side-by-Side: Side Effects of Ritalin and Adderall
As with any medication, Ritalin and Adderall both carry a range of potential side effects. They have several overlapping adverse reactions such as reduced appetite, sleep difficulties, and accelerated heart rate. Each can also cause distinct side effects which might affect choices in treatment. Sometimes the impact of Adderall is similar to that of Ritalin. How an individual reacts can differ significantly.
Common Ground: Similar Side Effects
Ritalin and Adderall can lead to a range of side effects, which may include:
Accelerated heartbeat
Headache episodes
Feelings of anxiety
Reduced hunger
Gastrointestinal upset
Dermatological reactions like rashes
Sleep-related issues
Decrease in weight
Feeling excessively active or agitated
Shaking or tremors
Tics development
Gastrointestinal changes such as diarrhea or constipation
Variability in mood
Appearance of hives
Difficulties sleeping
Frequent nervousness
Lightheadedness
Pain within the abdomen
Recognizing symptoms associated with potentially serious conditions like dangerously high blood pressure is essential. It’s important to consult with medical professionals if these signs become severe or do not subside.
Diverging Paths: More Serious Side Effects
Although the majority of adverse reactions to Ritalin and Adderall tend to be minor, there exists a potential for severe side effects. Individuals with pre-existing cardiac issues should be closely supervised due to warnings about infrequent but significant cardiovascular incidents associated with these medications.
Specifically, notable serious side effects from Ritalin include experiencing chest discomfort, difficulty breathing, and profuse perspiration. Meanwhile, Adderall may lead to elevated blood pressure and an accelerated heartbeat.
Navigating the Risks: Addiction and Withdrawal Symptoms
Adderall and Ritalin, when taken according to medical guidance, present a minimal risk of addiction. Nevertheless, if misused, dependence on both Ritalin and Adderall can develop along with associated withdrawal symptoms. It’s akin to walking into a bear trap—there isn’t significant danger in the action itself. Rather it lies in trying to free oneself from its grip.
Dependence Dilemma: Stimulant Medication Warnings
Although stimulant medications have a minimal risk of addiction, there is still a concern for possible misuse and the chance of becoming addicted, particularly in those who have previously abused substances. Hence, it is critically important to follow the prescribed medication dosage exactly as instructed by a medical professional.
Coping with Withdrawal: What to Expect
Typically, the withdrawal symptoms experienced from these medications are not severe. Those discontinuing may observe the following changes:
A heightened sense of tiredness throughout daytime hours
Enhanced capability for nocturnal sleep
A rise in hunger levels, especially if previously reduced by the medication.
Once an individual has stopped taking their medication, it might take a few weeks before their appetite returns to a stable level.
Delivery Methods and Dosage Forms: Ritalin LA vs. Adderall XR
Ritalin and Adderall, accommodating various therapeutic requirements, come in formulations that are both short-acting and long-acting. This range of options provides the capability to tailor treatment strategies to suit each person’s daily schedule and their ability to consistently adhere to medication protocols.
Short Acting vs. Extended Release: Choosing the Right Form
Formulations with extended release, such as Adderall XR and Ritalin LA, provide lasting symptom control using a once-daily dose. Conversely, for effective management of symptoms, short-acting drugs like Ritalin and Adderall might necessitate several doses during the day.
Choosing the most appropriate version depends on what fits well with your daily routine.
Generic Versions and Brand Names: Cost-Effective Options
When selecting medications for ADHD, financial considerations are often key. Fortunately, affordable options exist in the form of generic versions of ADHD drugs. These generics contain identical active components and adhere to the FDA’s stringent guidelines for bioequivalence, guaranteeing comparable therapeutic effects as their brand-name counterparts but at a reduced cost.
Maximizing Savings with NiHowdy’s Prescription Discount Card
Every penny saved is significant in controlling healthcare costs, and that’s precisely the advantage provided by NiHowdy’s prescription discount card. This isn’t merely a tool for achieving considerable savings on medications. It Rewards you with Bitcoin for each transaction you make! Indeed, this constitutes a dual benefit scenario we can all appreciate.
How NiHowdy Can Offset ADHD Treatment Costs
Regardless of one’s insurance status or income level, NiHowdy’s discount card enables users to obtain considerable savings on prescription medications. Specifically for ADHD treatment, this could translate into a reduction of up to $95 in the cost of ADHD medications—easing the financial strain and making managing ADHD more accessible.
The Added Value: Earning Bitcoin with Every Purchase
Imagine receiving Bitcoin rewards with every purchase you make using your prescription discount card. Imagine accumulating a digital currency that has the potential to appreciate in value over time, simply by utilizing your prescription discount card for routine purchases.
Think of it as stumbling upon a treasure chest amid your regular healthcare journey.
Summary
Navigating the world of ADHD medications can be challenging. With this guide, we hope you now understand the differences between Ritalin and Adderall, their side effects, and how to choose the right one for your needs. Remember, it’s all about finding what works for you. And with tools like NiHowdy’s prescription discount card, managing your ADHD treatment costs can be much easier!
Frequently Asked Questions
What is the main difference between Ritalin and Adderall?
Ritalin and Adderall, although similar in purpose, differ fundamentally in their chemical makeup. Ritalin is composed of methylphenidate, while Adderall consists of a mixture of amphetamine salts: amphetamine and dextroamphetamine.
Which one is more effective, Ritalin or Adderall?
The age of the patient plays a significant role in determining whether Ritalin or Adderall is more effective. While Ritalin tends to be better suited for young individuals, including children and teenagers, adults typically experience greater effectiveness with the use of Adderall.
Do Ritalin and Adderall have similar side effects?
Indeed, Ritalin and Adderall share several side effects including a reduced appetite, sleeplessness, and an elevated heart rate. Each has its own distinct set of adverse reactions as well.
It’s important to take note of these individual side effects when contemplating the use of either Ritalin or Adderall.
Can I become addicted to Ritalin or Adderall?
Indeed, if Ritalin or Adderall are misused, there is a risk of developing an addiction to these substances. This can result in dependency and the onset of withdrawal symptoms.
What is the NiHowdy’s prescription discount card, and how can it help me?
You can cut costs on medications and simultaneously accumulate Bitcoin for each acquisition by utilizing the NiHowdy’s prescription discount card.
Is Ritalin the Same as Adderall? Unpacking the Truth About ADHD Medications Read More »