Understanding the Timeline: How Long Does Lexapro Stay in Your System?
Understanding the Timeline: How Long Does Lexapro Stay in Your System?


Understanding “how long does Lexapro stay in your system” is crucial, especially if you’re considering discontinuation or are concerned about withdrawal. The elimination process depends on various factors, including metabolism and liver function. This article will explore the key elements that determine Lexapro’s presence in your body and offer guidance for those looking to taper off safely.
Key Takeaways
Lexapro (escitalopram) is an SSRI antidepressant that enhances serotonin levels and is commonly used to treat depression and anxiety, with a relatively fast onset due to its allosteric action.
The half-life of Lexapro ranges between 27-32 hours and factors like genetic enzyme variations, liver function, age, and body weight can influence its elimination rate, taking around 6.1 days for 99% clearance from the system.
Stopping Lexapro abruptly can lead to antidepressant discontinuation syndrome, therefore, a gradual tapering schedule under healthcare supervision is recommended to safely reduce withdrawal symptoms.
Lexapro Overview: What You Need to Know
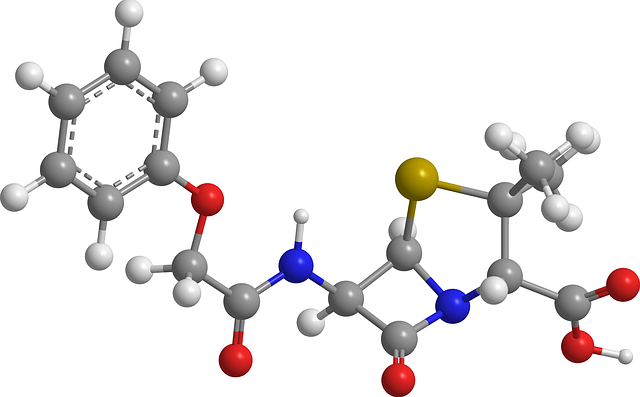
Escitalopram, commonly known as Lexapro, serves as a crucial aid for individuals suffering from anxiety and depression. This powerful antidepressant drug works to balance serotonin levels in the brain, offering relief and hope to those battling these disorders. It’s particularly favored among antidepressants due to its allosteric mechanism, which enables it to deliver results faster than other selective serotonin reuptake inhibitors (SSRIs), providing swifter relief of symptoms by enhancing the inhibition of serotonin uptake.
So what is behind Lexapro’s effectiveness? It falls under a class of drugs called selective serotonin reuptake inhibitors (SSRIs), which are frequently prescribed to manage both depressive and anxiety disorders. Let’s explore. What this entails.
Selective Serotonin Reuptake Inhibitors (Antidepressant Medication)
Antidepressant medications such as Lexapro are essential in managing major depressive disorder. Their mechanism involves:
obstructing the reabsorption of serotonin
elevating the amount of serotonin present at nerve junctions within the brain
improving communication between nerve cells
mitigating symptoms associated with major depressive disorder
alleviating intense anxiety.
These SSRIs come with their own set of challenges. Abrupt cessation or antidepressant withdrawal can trigger withdrawal symptoms known as antidepressant withdrawal. This raises an important concern. What is the appropriate method for safely discontinuing medications like Lexapro that treat major depressive disorder?
Prescribed Uses of Lexapro: Major Depressive Disorder (MDD) & Generalized Anxiety Disorder (GAD)
Lexapro has emerged as a pivotal ally for individuals grappling with major depressive disorder, providing significant relief. It serves as a beacon of hope, offering adults and children 12 years and older an escape from the depths of depression and guiding them towards a rewarding existence.
Lexapro plays an equally vital role in confronting generalized anxiety disorder (GAD) among adults and kids starting at age 7. In this arena, it is indispensable for those seeking to regain dominion over their lives and achieve tranquility.
Lexapro’s Half-Life and Elimination Process

Grasping the concept of half-life is crucial for understanding the duration Lexapro remains active in your system. Once ingested orally, Lexapro’s half-life typically spans between 27 to 32 hours – this duration reflects how long it takes for the drug’s concentration within the body to decrease by half. If you are on a course of taking Lexapro, expect around 6.1 days for nearly all (99%) of the medication to be purged from your system.
Now let us delve into what ‘half-life’ actually signifies and consider various elements that could influence the half-life of Lexapro. These topics will be examined. In subsequent sections below.
Half-Life Explained
The term ‘half-life’ of a drug denotes the period required for the concentration of that drug within the body to decrease by fifty percent. This measurement is unaffected by how much or how long the medication has been taken. Achieving steady levels of a drug in one’s system usually necessitates approximately five half-lives.
Although, individual variations can lead to substantial differences in reported half-lives for any given drug. In relation to Lexapro, it predominantly exits through hepatic pathways and its metabolism involves enzymatic actions from CYP2C19 as well as CYP3A4 in the liver.
Factors Affecting Lexapro’s Half-Life
A multitude of factors can affect the half-life and metabolism of Lexapro within the body, such as:
Individual genetic differences in CYP2C19, an enzyme essential for metabolizing Lexapro, which could alter how quickly it is broken down and its subsequent half-life.
The presence of other drugs or substances in your system that may interfere with how Lexapro is processed.
Age-related considerations since older adults typically process Lexapro at a slower rate.
The health status of your liver because compromised liver functionality can impact the breakdown efficacy of this drug.
Each factor contributes to determining the duration that Lexapro remains active within one’s system.
Age and hepatic health are significant determinants. Those who are older or have impaired liver function tend to exhibit an increased elimination half-life for Lexapro—often exceeding the usual span between 27 to 32 hours. There appears to be a potential reverse correlation between an individual’s weight and how long escitalopram (the primary component in lexipro) stays present: those with greater body mass may eliminate escitalopram more swiftly from their systems.
Side Effects and Withdrawal Symptoms
Lexapro, while often essential for those it helps, is not free from possible adverse effects. Every drug carries the risk of side effects and Lexapro is no exception. These can range in severity, including some serious ones. Ceasing intake of Lexapro might precipitate withdrawal symptoms that are both physical and mental in nature. These symptoms have the potential to become intense if one abruptly halts use of the medication.
So then, which specific side effects may arise when you stop taking your Lexapro? And what can be anticipated should you make a decision to discontinue its use? The subsections following will explore these matters starting with an examination of typical side effects associated with Lexapro.
Common Side Effects
Initiating treatment with Lexapro can result in common side effects, which include feelings of nausea, the onset of headaches, experiencing a dry mouth, increased sweating, difficulty sleeping or excessive sleepiness during the day. You might also feel unusually tired and lethargic.
To these more common discomforts are neuropsychiatric symptoms such as dizziness after starting Lexapro use. You may notice muscle stiffness or spasms accompanied by sensations resembling chills. Mental confusion can arise along depression symptoms with challenges in focusing your attention and impairments in memory function. Sexual complications caused by taking Lexapro could involve uncomfortable prolonged erections, hurdles regarding sexual performance including orgasm alterations and vaginal bleeding post-intercourse. There is potential for decreased interest in sexual activity that may persist over time. Physical manifestations might also encompass fluctuations in hunger levels while occasionally users describe electric shock-like experiences within their brain when on this medication. Bouts of dizziness not unlike those initially mentioned could occur together with elevated body temperature as well as changes both to sensory processing and urination patterns.
Antidepressant Discontinuation Syndrome
Should you be contemplating stopping Lexapro, it’s critical to understand the possible withdrawal symptoms that might arise. Typically starting within one to three days to few weeks following your final dose, these symptoms can persist for a few days up to several weeks. Physical manifestations of withdrawal may include changes in appetite, brain zaps, dizziness, fatigue, headaches and shifts in sensory experiences.
Mental health should not be overlooked as emotional effects such as anxiety, panic attacks and depression are significant factors during this period. Pay particular attention to flu-like symptoms alongside signs of depression.
Around 44% of individuals who cease taking Lexapro could experience issues including dizziness and muscle tension accompanied by chills. A carefully managed strategy with a healthcare professional is essential to reduce the likelihood of intense withdrawal reactions – here the half-life of medication becomes pertinent regarding the timing when symptoms appear.
With these considerations in mind, let us delve into strategies for safely tapering off from Lexapro.
Tapering Off Lexapro Safely
Ceasing Lexapro use should be done with caution and patience. A methodical decrease of the medication dosage, implemented as per a medical professional’s guidance, is key to mitigating the onset of withdrawal symptoms. Following a structured tapering plan can greatly reduce the harshness of these symptoms, providing your body with a smoother transition period.
Now let’s delve into what constitutes an effective tapering schedule and how one might effectively control withdrawal effects. The following subsections will address these topics in detail.
Tapering Schedule
The process of reducing Lexapro dosage typically unfolds over a span of several weeks, with each tapering phase ranging from two to six weeks or potentially longer. It’s imperative that this gradual reduction is closely monitored by a healthcare provider in order to effectively manage any withdrawal symptoms that may arise.
Individualized tapering schedules are crafted based on the patient’s specific experience with the medication, including how long they have been taking Lexapro and their current dose level. Emerging research indicates that patients may fare better when following an extended tapering schedule which progresses for several months beyond reaching the lowest therapeutic dose of antidepressant medication, promoting more favorable outcomes and greater ease in symptom management.
Managing Withdrawal Effects
In order to decrease the likelihood of experiencing withdrawal symptoms, it is advisable to gradually decrease the amount of Lexapro taken by making incremental adjustments over a period of time. Depending on how an individual reacts, this might mean modifying the pace at which you reduce your dose or lengthening the time between these reductions in order to control any withdrawal effects that may occur. Should symptoms present themselves following a dosage decrease of Lexapro, it could be necessary to return momentarily to one’s prior dose before resuming tapering with smaller decreases.
The duration of withdrawal symptoms varies among individuals. Many tend to see improvements within a span of three months. Implementing self-care strategies like ensuring adequate nutrition through diet, getting sufficient rest and sleep, partaking in regular physical activity and seeking support from family members or supportive groups can significantly alleviate symptoms and assist those who experience withdrawal symptoms in mitigating their discomfort.
To minimize potential discomforts during lexapro dosage reduction periods—engage consistently healthy lifestyle choices nourishing body’s needs effectively managing challenges arising throughout the discontinuation process.
Interactions with Other Substances and Medications
It is critical to be aware that when you are on Lexapro, it may have interactions with various medications or substances which could result in negative consequences. Such interactions can alter the drug’s potency and impact your well-being, with effects varying from slight to serious.
Now, let’s explore how Lexapro might interact with alcohol and different drugs in more detail in the upcoming sections.
Alcohol and Lexapro
If you are currently on Lexapro for your depression, it’s important to think twice before having that glass of wine or beer. Consuming alcohol while taking this medication can interfere with its effectiveness by upsetting the chemical equilibrium in your brain and could exacerbate symptoms of depression. In severe cases, combining alcohol with Lexapro has been known to trigger aggressive behavior.
That said, some individuals may still be able to enjoy a moderate amount of alcohol when prescribed Lexapro. Typically, up to two drinks per day for men and one drink per day for women is considered within safe limits. Confirming this with your healthcare provider is essential as they can provide guidance on achieving an appropriate balance between treatment and lifestyle choices.
Drug Interactions
When taking Lexapro, it’s crucial to be aware of its possible interactions with other substances that can escalate side effects or even cause dangerous drug reactions. Drugs and supplements known for such risks when combined with Lexapro include:
MAO inhibitors: A combination of these drugs with Lexapro is highly risky and could result in a deadly interaction.
Tryptophan: Adding tryptophan supplements to your regimen while on Lexapro may amplify the chances of experiencing serotonin syndrome.
St. John’s wort: This herbal supplement, when used concurrently with Lexapro, increases the likelihood of triggering serotonin syndrome.
Before initiating treatment with prescribed lexapro, consulting your doctor or pharmacist is essential to discuss all current medications and dietary supplements you’re using. This ensures prevention against adverse interactions.
Certain heart rhythm modulating drugs like amiodarone and quinidine might have negative interactions if taken alongside lexapro. Moreover, drugs processed by the CYP2D6 enzyme (e.g., aripiprazole and atomoxetine) are particularly prone to increased side effects due to higher concentrations in the body caused by concurrent use of lexaprо.
Summary
In essence, Lexapro serves as an effective aid in treating major depressive disorder and generalized anxiety disorder. Knowing the duration of its presence within your system, including its half-life and influencing elements, is essential. It’s imperative to be cognizant of possible side effects and withdrawal symptoms, underscoring the necessity for a carefully planned tapering schedule. Being alert to how it may interact with substances such as alcohol or other drugs is crucial for ensuring safety during use. Although overcoming these challenges can be difficult, armed with proper understanding and support systems in place, one can approach recovery from mental illness with assurance.
Frequently Asked Questions
What is the half-life of Lexapro?
The half-life of Lexapro ranges from 27 to 32 hours after oral administration, meaning it takes this amount of time for the drug level in the body to reduce by 50%.
What are some common side effects of Lexapro?
Be aware that when taking the medication Lexapro, typical side effects may occur such as feeling nauseated, experiencing headaches, having a dry mouth, sweating excessively, suffering from insomnia or drowsiness, battling fatigue and encountering sexual side effects.
It is important to keep these potential reactions in mind while using this medication.
What are the symptoms of Lexapro withdrawal?
If you encounter symptoms such as changes in appetite, sensations akin to ‘brain zaps’, dizziness, tiredness, headaches, shifts in sensory experiences, anxiety or depression during withdrawal from Lexapro, it is crucial to consult with your doctor or your healthcare provider.
How can I safely taper off Lexapro?
When discontinuing Lexapro, it is crucial to gradually reduce the dosage in incremental steps. Ensure you are under the careful guidance of a healthcare provider throughout this tapering process for safe management.
Can I drink alcohol while taking Lexapro?
Steer clear of consuming alcohol during your Lexapro treatment since it may diminish the medication’s potency and exacerbate symptoms of depression.
Should you have any questions or issues, reaching out to your healthcare provider is crucial.
Understanding the Timeline: How Long Does Lexapro Stay in Your System? Read More »