Understanding Bipolar 1 vs 2: Navigating the Key Differences


Are you confused by the differences between bipolar 1 and bipolar 2 disorder? Bipolar I is notorious for its intense manic episodes, while Bipolar II is characterized by less severe hypomania combined with serious bouts of depression. This article will guide you through their defining features, their impact on daily life, and how each is managed. Expect an insightful walkthrough aimed at demystifying these complex disorders for those who experience them or seek to understand them.
Key Takeaways
Bipolar I is characterized by at least one full manic episode, which may lead to psychosis, whereas Bipolar II involves less severe hypomanic episodes paired with recurrent depressive episodes, differing not in severity but in episode types.
Diagnosis of bipolar disorder is a multi-step process including a physical exam, mental health assessment following DSM-5 criteria, and careful consideration of patient history to accurately identify the subtype (Bipolar I or II) based on manic or hypomanic episodes.
Treatment of bipolar disorders typically involves a combination of medication (mood stabilizers and antipsychotics) and psychotherapy (like CBT), complemented by lifestyle modifications (routine, stress management) and strong support networks with family, friends, and peer groups.
Exploring Bipolar I and Bipolar II Disorders

The bipolar spectrum is primarily defined by two subsets, known as Bipolar I and II. Each subtype displays common patterns of mood variation but also has unique features that distinguish them from one another. Recognizing these differences is crucial as they are fundamental in crafting targeted treatment plans and providing appropriate support for those with either condition.
In the case of Bipolar I disorder, individuals encounter severe manic episodes marked by significantly heightened moods and increased energy levels. Conversely, Bipolar II disorder involves milder hypomanic episodes paired with repeated depressive episodes. The distinction between Bipolar I and II hinges not on a gradient of severity but on the specific nature of the mood episodes experienced within each category.
Defining Bipolar I: The Intensity of a Manic Episode
Examining Bipolar, I disorder more closely; it is defined by the occurrence of at least one manic episode. These episodes can persist for a week or longer or be intense enough to necessitate hospital admission, typically causing significant disturbances in life. Symptoms such as accelerated speech patterns, an onslaught of rapid thoughts, and diminished sleep requirements are common. Such symptoms frequently precipitate engagement in behaviors that may carry risks, like rampant spending sprees or participation in risky activities.
In contrast to Bipolar II, the heightened severity of manic episodes within Bipolar I disorder stands out distinctly. These full manic episodes have the potential to escalate into psychosis, where individuals lose their grasp on reality—an extreme manifestation not seen with hypomanic episodes associated with Bipolar II disorder.
Understanding Bipolar II: Hypomania and Depression
Bipolar II disorder is similar to bipolar I but differs in that it involves milder hypomanic episodes coupled with significant periods of acute bipolar depression. During a hypomanic episode—which lasts for at least four days—individuals may experience an elevated mood, heightened talkativeness or fast-flowing thoughts, increased energy and spontaneity, along with potentially harmful behaviors and tumultuous personal relationships.
The frequent occurrence of depressive episodes can often result in the misidentification of bipolar II. It’s common for people to seek treatment predominantly when experiencing these lows. Hence, mental health professionals must diligently assess any history of hypomanic behavior. A correct diagnosis hinges on recognizing not just recurrent bouts of depression but also identifying the existence of at least one previous hypomanic episode indicative of Bipolar II disorder.
The Spectrum of Mood Episodes in Bipolar Disorders

Within the intricate landscape of bipolar disorders, individuals encounter a range of mood episodes, from the extreme highs associated with Bipolar I to the profound lows that are characteristic of both types. The manifestation and progression of these episodes differ widely among patients in terms of number and intensity, illustrating how diverse and nuanced bipolar disorders can be and underscoring the importance of tailored approaches to treatment.
In this broad spectrum of mood disorders lies an intriguing element known as mixed episodes. These occur when characteristics typical for mania blend with depressive symptoms concurrently within one person, referring collectively to manic and depressive episodes. Those living with bipolar disorder must become adept at recognizing their unique precursors and warning signs—such as changes in sleep patterns or eating habits—to effectively navigate their illness through proactive management and prompt action when necessary.
The Highs: Manic Symptoms in Bipolar I
Manic episodes within Bipolar I Disorder are distinguished by a mood that is excessively elevated, expansive, or irritable for at least seven days. Other hallmarks of these episodes include an extraordinarily high energy level, accelerated speech patterns, thoughts that race uncontrollably, and the need for less sleep than usual.
Such intense manic phases typically lead individuals to pursue pleasurable activities without considering the possible negative consequences or disruptions they may cause in their lives.
Bipolar I disorder stands apart as a mental illness, mainly because during its manic episodes, there is a higher chance of experiencing psychosis. When this occurs, the person’s connection with reality becomes compromised, which highlights how severe symptoms can be when compared to hypomanic episodes seen in those with Bipolar II. Recognizing such distinctions between these disorders regarding symptomatology and impact is vital.
The Lows: Depressive Symptoms Across Bipolar I and Bipolar II Disorder
Conversely, depressive episodes manifest as profound sadness, feelings of inadequacy, and diminished interest in once-enjoyable activities. Such episodes are characteristic of both forms of bipolar disorder—not solely Bipolar II—and bear a striking resemblance to those seen during major depressive episodes: intense sorrow, fluctuations in appetite and sleep patterns, and challenges focusing.
It’s critical to acknowledge that despite the often more extreme reputation due to its manic spells, Bipolar I disorder also shares these distressing periods. In cases of Bipolar II, an individual may experience these debilitating phases more frequently and for longer durations, which can seriously disrupt day-to-day life both socially and professionally—underscoring the complexity inherent in treating Bipolar II effectively.
Diagnosing Bipolar: A Critical Step for Effective Management
The process of diagnosing bipolar disorder encompasses various steps, such as:
Undertaking a physical examination to exclude any other possible medical issues
Conducting an in-depth evaluation of mental health using the criteria outlined in the Diagnostic and Statistical Manual of Mental Disorders (DSM-5)
Identifying which subtype of bipolar disorder is present
Such measures are essential for reaching an accurate conclusion when distinguishing between bipolar disorder and other similar conditions.
At the heart of this diagnostic protocol lies meticulous scrutiny and analysis regarding the individual’s historical behavioral patterns, incorporating discussions with the patient and potentially their close associates or family members. The goal here is to pinpoint an exact diagnosis by identifying if there have been incidence(s) that constitute what would be termed as a full manic episode according to established guidelines.
Treatment Approaches for Bipolar I vs Bipolar II

Upon unlocking the complexities of bipolar conditions, it’s essential to delve into the diverse therapeutic strategies for managing both Bipolar I and II disorders. Such management usually comprises a personalized regimen combining mood stabilizers, antipsychotics, and antidepressants—adjusted according to individual symptoms. Psychotherapy is also integral in successfully navigating symptom control.
Notably, individuals with Bipolar II often exhibit a more gradual response to treatment interventions than their counterparts with Bipolar I disorder. After eight weeks, those with either type of bipolar disorder typically demonstrate comparable improvement levels in their condition. This highlights the necessity for ongoing commitment and perseverance in treating bipolar disorders effectively.
Medication Strategies: Stabilizing Mood Swings
Pharmacological interventions serve as a pivotal strategy in the treatment of bipolar disorder, providing a navigational aid to individuals battling relentless mood fluctuations. Key pharmaceutical agents employed include mood stabilizers such as lithium and valproic acid, complemented by antipsychotic medications like olanzapine, risperidone, and quetiapine.
Determining the most suitable medication—whether it be mood stabilizers or antipsychotics—is an individualized approach that hinges on the patient’s specific symptomatology. Careful consideration is imperative when incorporating antidepressants into the therapy regimen to mitigate the potential for inducing manic episodes.
Psychotherapy and Support: Navigating Mental Health Challenges
Psychotherapy is an essential component of treating bipolar disorder, complementing medication. One therapy approach, cognitive behavioral therapy (CBT), enables those afflicted to substitute negative thought patterns with more constructive ones. Social rhythm therapy also plays a significant role in helping patients develop regular schedules crucial for stabilizing their moods.
Forming a robust support network is an essential strategy in managing bipolar disorder. Such networks can include family members, friends, or trusted individuals who offer emotional support and practical help when needed. Engaging with peer groups, either through local communities or online platforms, provides opportunities for sharing experiences and emotional solidarity among people living with bipolar disorder. This camaraderie helps alleviate feelings of loneliness by fostering connection and community.
Living with Bipolar Disorder: Lifestyle Modifications and Coping Strategies

Living with bipolar disorder involves more than just medication and therapy; it requires significant lifestyle modifications and coping strategies. Some fundamental lifestyle changes to consider include:
Maintaining a steady routine
Managing stress
Planning for potential crises
Following a regular sleep schedule
Identifying personal triggers
These changes can help stabilize mood and manage symptoms of bipolar disorder, as evidenced by placebo-controlled clinical trials.
Support from family and friends is also vital for managing bipolar disorder symptoms effectively and maintaining an individual’s quality of life. Combining lifestyle modifications with a strong support network is essential to navigating daily life with bipolar disorder. This approach provides a comprehensive strategy for managing bipolar disorder rather than relying solely on medication.
The Role of Routine: Managing Sleep Patterns and Daily Activities
Establishing a regular schedule is crucial in the management of bipolar disorder. Using social rhythm therapy, patients can create and maintain a steady daily pattern to aid in the stabilization of their mood fluctuations. Adhering to such routines may grant individuals with bipolar disorder greater steadiness by instilling tranquility during elevated moods and offering encouragement when experiencing depressive states.
Maintaining physical health through adequate sleep, nutritious eating habits, and consistent exercise contributes positively to mental health for those managing bipolar disorder. Incorporating relaxation techniques, engaging hobbies, and social activities into one’s everyday regimen promotes balance for people with this condition. It’s akin to charting out a predictable course through the complex maze that is bipolar disorder—minimizing unforeseen diversions that could exacerbate symptoms.
Building a Support Network: Engaging Family and Healthcare Providers
Creating a support system is akin to assembling a team of navigators for the complex journey through bipolar disorder. Enlisting friends, family members, or other trusted individuals in this group can provide emotional solace, practical help, and a valuable sense of community. For those with bipolar disorder, peer support accessible via online platforms or local organizations delivers mutual understanding and shared experiences, which alleviate feelings of solitude.
Family members and companions are pivotal in helping manage bipolar disorder.
Recognizing preliminary indicators of mood episodes
Supporting adherence to self-care routines
Maintaining an open conversation about beneficial strategies
Following advice from mental health professionals
This concerted action underscores the adage that raising a child requires communal involvement—similarly, managing mental health conditions like bipolar disorder benefits greatly from collaborative efforts.
Financial Assistance for Bipolar Disorder Treatments
Embarking on the path through the bipolar maze is not solely a psychological and emotional endeavor. It equally encompasses economic implications. The expenditure for medications tailored to treat bipolar disorder can be significant, thus making fiscal support a crucial element in managing this condition. Prescription discount cards are invaluable because they grant notable reductions at pharmacy counters.
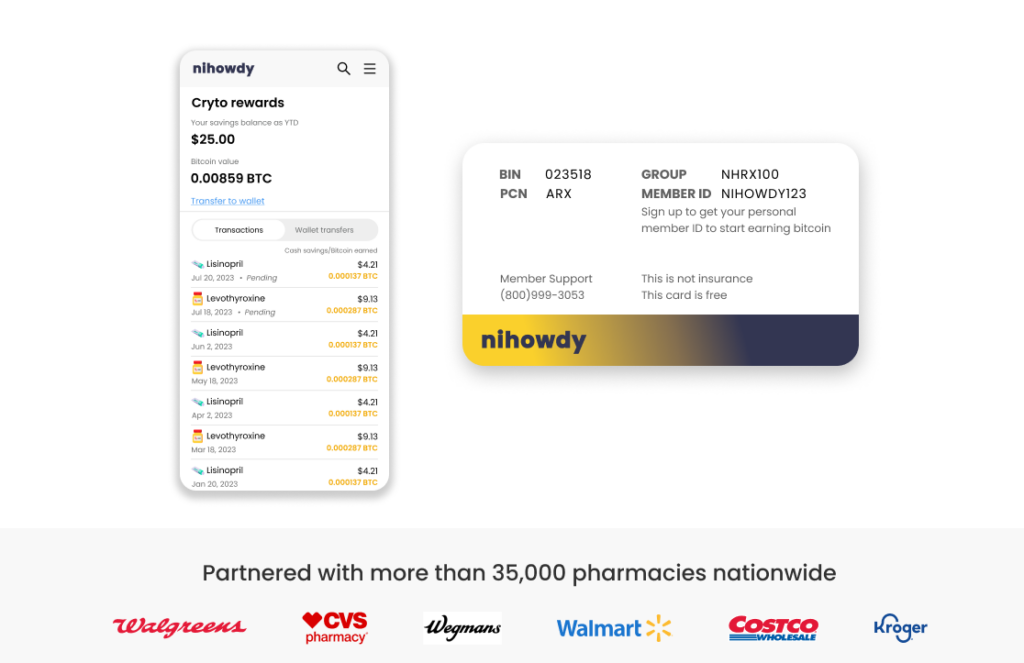
The NiHowdy prescription discount card epitomizes such a tool. It grants immediate discounts at pharmacies and incentivizes individuals with Bitcoin rewards upon each refill of their prescriptions, aiding in mitigating escalating healthcare expenses.
NiHowdy’s Prescription Discount Card: Maximizing Savings
The NiHowdy prescription discount card provides several advantages.
Immediate cost reduction at pharmacy counters.
Rewards its users in Bitcoin for every prescription they refill.
Offers prompt financial relief on medication expenses.
The returns from using the NiHowdy’s card have the potential to increase over time, yielding significant benefits.
Over an extended period, the rewards accumulated through NiHowdy’s complimentary program may help counterbalance escalating healthcare expenses or assist with other significant financial outlays.
Summary
Embarking on the exploration of bipolar disorder is akin to traversing a labyrinth replete with complexities and nuances. Delving into the spectrum of mood episodes, discerning the key differences between Bipolar I and II disorders, dissecting diagnostic criteria, scrutinizing treatment methodologies, contemplating lifestyle adjustments, and addressing economic support mechanisms have been an illuminating yet intricate process.
Amidst this seemingly convoluted realm of bipolar disorder lies reassurance that through comprehension, guidance, and communal solidarity, one can adeptly steer through its intricacies. You stand not in isolation. Armed with pertinent resources and strategies, you are empowered to control bipolar disorder effectively while pursuing a life rich in satisfaction.
Frequently Asked Questions
What are the critical differences between Bipolar I and II disorders?
Bipolar I and II disorders are differentiated by the intensity and nature of mood episodes they entail. While Bipolar I is associated with complete manic episodes, Bipolar II is distinguished by recurrent depressive episodes coupled with hypomanic episodes that are less severe than those observed in Bipolar I.
How are manic episodes in Bipolar I different from hypomanic episodes in Bipolar II?
In Bipolar I, the manic episodes experienced are typically more intense and prolonged compared to the hypomanic episodes characteristic of Bipolar II, which can result in considerable interference with daily life and sometimes dangerous actions.
What is the role of medication in the treatment of bipolar disorder?
In the management of bipolar disorder, it is crucial to utilize medications like mood stabilizers and antipsychotics. These drugs are vital in controlling symptoms and thwarting subsequent mood episodes, forming a foundational component of the comprehensive treatment strategy.
How important is lifestyle management in managing bipolar disorder?
Maintaining a consistent daily schedule and ensuring regular social interaction are essential components of lifestyle management that play a vital role in stabilizing mood swings and effectively handling the symptoms of bipolar disorder.
What financial assistance is available for managing bipolar disorder?
Utilizing prescription discount cards is a smart move to reduce the expense of medications. The NiHowdy prescription discount card significantly reduces pharmacy checkouts and rewards you each time you refill a prescription.
For those dealing with the financial aspects of bipolar disorder treatment, leveraging such cards can be highly beneficial in mitigating costs.